|
Public health advice and directives are required to be evidence-based, but also are urgently needed in real time, during pandemics. Statements, often used to evaluate policy options, have been made about the SARS-CoV-2’s testing, origin, infectiousness, contagiousness, severity, and evolving variants, as well as the many ways to combat the virus’ impacts through population- to individual-level approaches such as mask wearing, social distancing, vaccination, convalescent plasma treatment, antivirals and steroids. It is useful to review the inherent limitations of commonplace statistics and analyses and approaches in the ongoing fight against SARS-CoV-2. This unmasking is not meant to debunk myths, but rather to highlight the nuanced world we live in with respect to testing for epidemiological outcomes of interventions or ascribing treatments of Covid-19 as efficacious or effective. Below, I share three of the best treatments about the limitations of statistics in this early age of coronavirus.
Testing for the virus: sensitivity and specificity A first step in dealing with a contagious and severe disease is knowing which individuals are infected, so as to isolate them and quarantine their contacts. Let’s say 1% of 100000 tested are actually infected, but 95% of the time our test returns a positive test result for an infected individual. Then, ~50 out of 1000 infected persons score as being uninfected or are false negatives. For a virus with superspreading potential, it would not be very useful to tell 50 people that they are uninfected when, in fact, they are infected. We also can consider the specificity of the test or the likelihood of returning false positives at 5%. Here, ~4950 of 99000 individuals test positive for the virus when, in fact, they were uninfected. Our estimate of % of individuals infected is therefore 950+4950 or ca. 5.9% -- well above the actual 1% infected. The main point here, which can be shown with additional math, is that the estimate of % infected upon which case rates are based depends on the test’s sensitivity and specificity, but also on the background level of infection —which we do not actually know. These factors likely vary from test to test, place to place and time to time. Estimating the % infected depends on our combining tests using various methods, retesting often, and assessing clinical symptoms. Using those data in analyses depends on our being clear about how the outcomes were derived (see Waltner-Toews 2020 for a treatment of this and related problems during pandemics).1 Vaccine efficacy and effectiveness Vaccine efficacy rates and vaccine effectiveness are different, as discussed in the excellent backgrounder, posted in Vox. The problem is that vaccine efficacy rates might not reflect their effectiveness. Vaccine efficacy rates are derived from comparing the newly infected cases ascribed to the vaccinated groupvs. ascribed to the placebo group. Say, for example, 100 people got infected after a period of time involving following thousands of vaccinated and placebo participants in a clinical trial. If each group had the same numbers of participants ‘treated’ at the outset and if 75 of the infected individuals were in placebo group and the remaining 25 infected individuals in the vaccinated group, then non-vaccinated participants were 3X more likely to get Covid-19. Vaccine efficacy is context (or trial) dependent because these statistics depend on when and where trials were conducted. Let’s say background case rates are high, possibly due to a highly infectious or highly transmissible variant of concern. In this scenario, even vaccinated individuals might become infected often, possibly before vaccines take effect or from multiple exposures. Such a scenario would depress estimates of vaccine efficacy rates with respect to infection likelihood. From an individual health standpoint, however, it is much more important to address the vaccine’s effectiveness— how the infected individuals fared in each group with respect to having mild to moderate symptoms vs. individuals experiencing severe symptoms of the virus and requiring hospitalization. This comparison is less likely to be context dependent as only severe cases are likely to be hospitalized across districts. So, comparing rates of hospitalizations among infected individuals from vaccinated and placebo groups can be a rigorous way to assess the protection against disease severity as afforded by vaccines. The different vaccines are currently all near completely effective in protecting against severe Covid-19 disease. The (false) promise of ecologic (or aggregate) studies Ecologic studies were rampant during the early days of Covid-19 and are still ongoing. Basically, these types of studies rely on comparisons of populations (often aggregated at the level of country) that vary in Covid-19 case or mortality rates and which also vary in key attributes. The thinking is that factors that explain statistical variation in Covid-19 case or mortality rates at the aggregate level might also be important at the individual level and might lead to beneficial interventions. Ecologic studies are best thought of as hypothesis-generating exercises and, at worse, a complete waste of a limited investment of time by researchers. But the results of ecologic studies can be appealing and do take up media bandwidth. There is a brief “Skeptic’s guide to ecologic studies during a pandemic” posted roughly a year ago in Forbes magazine that does an excellent job of outlining the limitations of ecologic studies in general and, more specifically, with respect to Covid-19. This post has heaps of wisdom in it and should be read by everyone interested in epidemiology and global health. One of the inherent problems with ecologic studies is that chasing leads can result in opportunity costs, as noted in the Skeptic’s guide. There might be promise with ecologic studies, but their utility will depend on a rigorous dose of epidemiological thinking at the outset, careful consideration of potential confounds and precision of outcome measures, and a healthy reticence to just hack through minefields of big data. Considering these three broad examples and their sources: testing for the virus, testing for vaccine efficacy and effectiveness, and ecologic testing of potential determinants of Covid-19 case and mortality rates, should be sufficient to introduce the limitations of statistics. Whether or not the statistical approaches used to address Covid-19 related phenomena are worthy of attention (or worthless) depends on knowing the context in which they were generated and ultimately cited. The above sources have all implied or stated explicitly that it is crucial to get the science and analysis right, especially during crises. To achieve this, we have to be neither ignorant of, nor apathetic toward, the statistics, but embrace them for what they can tell us. ------ 1, Waltner-Toews, D. 2020. On pandemics: deadly diseases from bubonic plague to coronavirus. Greystone Books Ltd. Vancouver, 262 pp.
0 Comments
Ontario, like many other jurisdictions around the world, was caught off-guard by CoViD-19. As soon as the cases and then the deaths mounted, policy frameworks were established to shut down the economy and lockdown the mobility of Ontarians. Emphasis was placed on the hotbeds of the pandemic: long term care facilities.
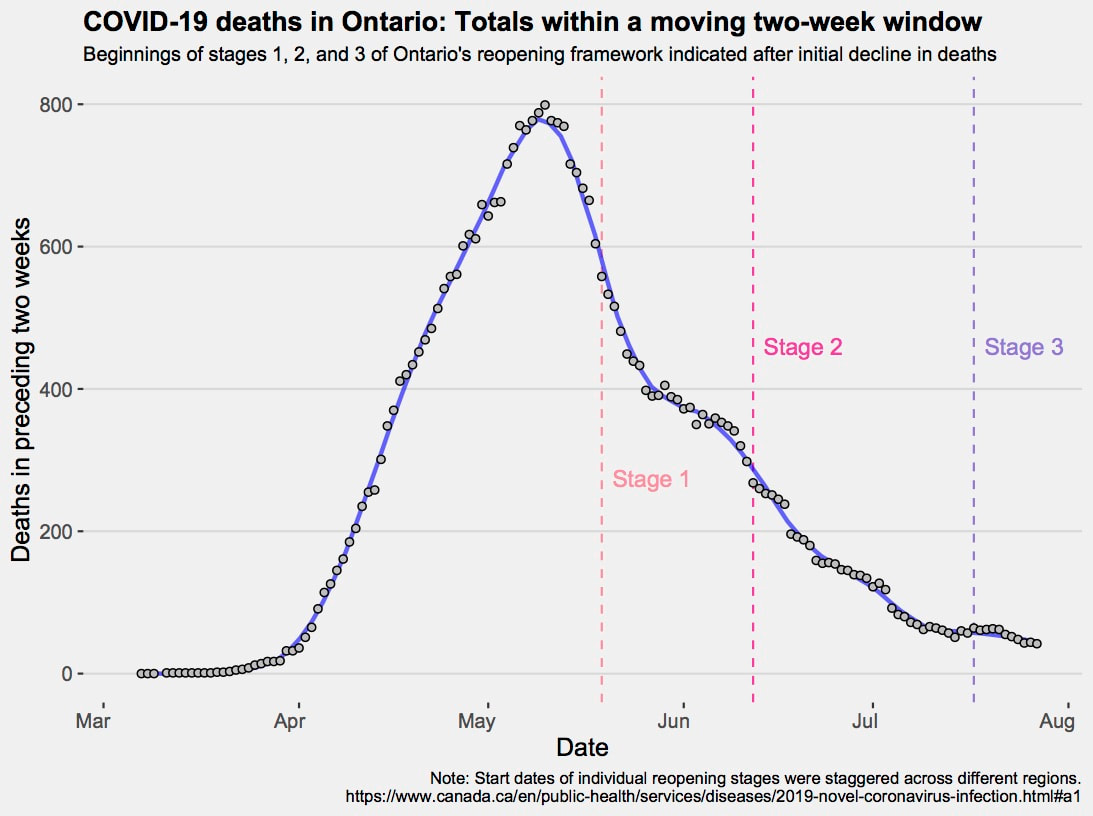
For society as a whole, best practices, given the evidence, were soon enacted. First, came the social distancing and handwashing, then the restrictions on size of social bubbles and the use of face masks mainly for indoor gatherings. All of this has been at a cost of our collective mental health. We are, after all, social animals. Soon after the ‘safety-first’ measures were implemented, debates surfaced for a quickened versus gradual re-opening of societies. Calls for widespread testing for the virus, and antibodies to it, were made to scope out the context-dependent epidemiology of SARS-CoV-2 and to get intel on whether re-opening of schools, businesses, and government offices was warranted. But such tests are known to be problematic due to false negative and false positive rates, and also because the numbers of coronavirus cases uncovered relates to testing effort. More testing necessarily means more cases revealed, which is a problem if uncorrected case numbers are used to project a disease’s trajectory. Below, we plot the 2764 tragic deaths of Ontarians from CoViD-19 as previous 2-week rolling totals (each day from the epidemic’s start up to and including 27th July). We mark the initial stages of Ontario re-opening – differences in regional re-open start dates were mandated by the government. The graph shows a current smouldering of infections and a higher background rate of mortality than seen at the epidemic’s start, suggesting it is too soon to relax guards. Remarkably, the first peak of mortality has passed, and decisions to gradually re-open Ontario were coincident with an ever-dwindling mortality. Trends like these can be used as evidence supporting decisions to cautiously rejig society. The smoothed mortality totals are less subject to the vagaries of sampling compared to case rates, but they might also be subject to disparities in realized health care capacity or reporting, when compared between jurisdictions. A recent tweet by a Carleton University PhD graduate, Dr. Jenn Provencher, said something to the effect that Indigenous people are willing to share traditional knowledge, if they think you are willing to learn. She was live tweeting at the Annual General Meeting of the Association of Canadian Universities for Northern Studies (ACUNS) and was sending to twitter a paraphrase of one of the keynote’s, Sen Murray Sinclair’s, inspirational points. So true! For our work on avian cholera in the Arctic, Inuit participation, guidance, and direction was of paramount importance. Collectively, it steered another Carleton PhD candidate, now Dr. Sam Iverson, to many eider duck breeding colonies on islands along the shores of Hudson Strait.
Parasites are aggregated, but how are contaminants distributed among the hosts? And why does it matter?
A recent paper by André Morrill, Jenn Provencher and myself recently asked and partially answered these questions. We reviewed the literature over 23 years to show that interest in the combined effects of contaminants and parasites on host health was increasing exponentially. In actual fact, the studies were of three main types: one type was the extent to which parasites bio-magnify the contaminants of their hosts. This effect of such parasites on contaminant burdens in hosts may well have host health effects. Much to build on there! Why parasites (typically intestinal helminthes are studied) even do such a thing is fascinating? There has been some intriguing research on the potential links between peanut allergies and antibiotic use early in life. Two labs in the United States appear foremost in this research area. One is at the University of Chicago and the other is at New York University. The work by Dr. Nagler and her team have shown that the removal of Clostridia bacteria might be responsible for sensitization to peanut allergen, in a mouse model. Mice models are useful because researchers can document clinical signs of allergy. But the interesting result was that the presence of the Clostridia bacteria appears responsible for gut inflammation that reduces the rate at which the peanut allergen is absorbed into the blood. Other research by Dr. Blaser (Missing microbes fame) at NYU is suggesting that missing microbes may be important in several health issues (rogue bacteria, food allergies). These are exciting directions for future research.
I was walking on the weekend when I came across this little amphibian. Many of you will have recognized this as a red eft the terrestrial stage of a salamander species common to this neck of the woods (or at least to ponds therein).
Note the following blog was written before I knew about the research highlighted in another blog: see "Did rats spread the black death?" Anyway, with that caveat, you can still read my wiki thoughts on the plague, starting now…
I recently saw a serial called Spiral on Netflicks (an engaging crime drama set in France) wherein one of the episodes a judge intoned something to the effect that the lesser of two evils was itself still quite an evil. Loosely translated the statement was “it’s cholera or it’s the plague”. It got me doing a sort of imagining what it must have been like to live during one of the outbreaks of bubonic plague in Europe, while at the same time tasking by queuing up the next episode of Spiral (this episode featuring a cop with a drug addiction). To help with the former, I turned to the digital milieu of Wikipedia. I am going to go out on a limb and suggest that many, if not most, parasite species exploit several to many hosts species, for a given stage of their (i.e., the parasite’s) life cycle. The question of why such parasite species are catholic in their diet (I say diet because, really, the host is a source of food for the parasite’s growth, development and/or reproduction), remains largely an open question. One interesting nuance is that a given species of parasite often has differential fitness or success on different host species (here, we are controlling for time and location of collection of both the parasite and host species). A troubling issue is why the parasite has not evolved discrimination, another is why some host species are better hosts than others, a third is whether there are alleles coding for host species use that are in competition with one another. There are several other questions such as how important is host species relative frequency across space and time in determining whether it is a principal species exploited by the parasite and what, if any, trade-offs exist in using one species over another. We are just starting to get answers to these questions. Sometimes, nature pitches real oddities at you. Consider, two damselfly species where one is totally susceptible to a mite ectoparasite and the other is totally susceptible. If you want to getthe scoop, visit Julia Mlynarek’s blog: Julia was one of my PhD students here art Carleton University.
Recently, one of my former students, André Morrill, got a paper accepted in the Canadian Journal of Zoology as first author on explaining covariation between ectoparasitic mites and endoparasitic eugregarine protozoans of Lestes damselflies. Many previous researchers have addressed the extent to which either mites or gregarines are associated with reduction in fitness of their insect hosts. In these singular studies examining just one parasite taxa or species, there is the implicit assumption that any patterns discovered are attributable to the parasite under study, and not some other parasites species that has not been monitored or enumerated. André’s work shows that there are reasons to expect these parasites might covary. The link to the paper for those interested can be found here. André also has recently senior authored a paper in International Journal of Parasitology concerning how a Poisson distribution of random parasite encounter and a normal distribution of host condition can combine through a few simple rules of condition-linked immunity to produce the oft-seen and oft-cited negative binomial distribution of parasites on hosts. This research suggests that we need not invoke environmental heterogeneity in parasite infective stages to explain aggregated distributions on hosts; such occurrences, however, will make parasite distributions even more aggregated. Read the abstract of that paper here.
Recently, Sam Iverson got a lot of press on one of his PhD papers coming from the lab. In brief, polar bears are visiting seabird colonies and eating eggs more and more as sea ice is disappearing. The strength of Sam’s analysis lies in his expanding the geographical extent of what previously was thought to be anecdotal observations. For the full story, click here.
|
AuthorProfessor & student Archives
April 2021
Categories |

 RSS Feed
RSS Feed
